Many babies still in hospital, while respiratory season in Hungary is petering out

Key findings:
- 38.1%) of the samples tested on the 11th week of 2025 showed infection with some kind of influenza virus; down from 48.6% a week earlier;
- the influenza positivity rate for all samples tested (29.5%) continues to exceed the falling cumulated Covid positivity rate (6.8%), while the flu rate never took the lead in the 2023/24 season;
- the positivity rate for the respiratory syncytial virus (RSV) dropped for the first time (to 11.1%) since the 4th week of 2025;
- the number of human metapneumovirus (HMPV) infections reached 144 or 1.9% of all samples tested up to the 11th week, which figures compare with 102 and 1.7% a year earlier;
- the number of people hospitalised with severe acute respiratory infection (SARI) dropped almost 15% w/w to 274 from 322, which is higher the comparative figures in the 2023/24 (162) and 2022/23 (269) respiratory seasons;
- two people among the SARI patients tested positive for COVID-19, while there were 56 people with influenza infection in hospital (down from 94), which corresponds to 20.4% of all SARI patients (down from 29.2%); and 72 people were treated in hospital with RSV infection (down from 79, but up from a percentage of 24.5% all SARI patients a week eaerlier);
- of the 274 people in hospital with SARI, 97 (35.4%) were aged two years or younger, against 119 and 37% on the 10th week, while 106 (38.7%) were aged 60 years and older, up from 101 or 31.4% on the previous week.
Epidemic retreating for the second week in a row
The lower number of GP visits with respiratory infections and the epidemiological pattern of previous respiratory seasons suggested five weeks ago that the peak might have been reached. We were wrong, as the data for the following two weeks showed.
There seemed to be a turnaround on the 9th week, and the subsequent data confirmed that the worst of the epidemic is behind us, although the improvement was sluggish at first, but it accelerated on the 11th week. The number of people seeking medical help with acute respiratory infections (ARI) was 255.600, down 12.3% w/w, and the number of patients with influenza-like illness (ILI) fell sharply by almost 25% w/w to 55,200.
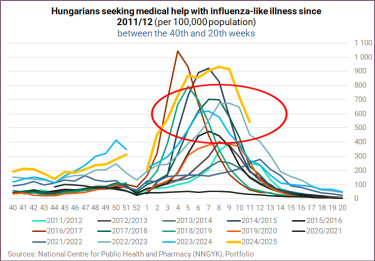
The respiratory season (often and erroneously referred to as 'flu season') generally peaks between the 4th and the 9th week of the year, so this year is not an outlier in this respect.
A short-term comparison (for the last three seasons of respiratory illnesses) shows that the number of patients with ARI, including those with ILI was higher than at this point in the previous two respiratory seasons.

The share of influenza-like illness in ARI was down at 20.3% from 23.7% on the previous week, exceeding the comparative readings from the past two seasons (13.4% and 19.9%, respectively), meaning that a fifth of ARI patients showed symptoms of influenza.

We also have data for ARIs and flu-like symptoms per 100,000 inhabitants, although a long-term data series is available only for the latter.
The current situation is worse than either of the previous two respiratory seasons in terms of both ARI and influenza-like illness per 100,000 people.


In the graph below, you can compare the flu situation with the previous 13 respiratory seasons and see that the situation has not been as bad as it is now.
One and a half months ago, the NNGYK reassured us in response to our enquiries that they "keep a close eye on the rate of serious illness", and drew the conclusion that with a low percentage of all patients requiring hospitalisation, the virus circulating was not causing more severe illness than we are used to.
By the 11th week, the ratio dropped a tad to 0.107% from 0.111%, coming in between the 2022/23 value of 0.121% and last year's 0082%. You find more detailed information about the situation in hospitals below.

Positivity rates
The influenza positivity rate (38.1%) has dropped after rising for two weeks, while the RSV positivity rate (11.1%) has fallen for the first time since the 4th week, and remains higher than on the 11th week of either of the last two respiratory seasons.


The following graph may seem a bit fuzzy at first but at least it shows a side-by side comparison of the weekly positivity rates for influenza (green), Covid (orange), and RSV (blue) for the past three respiratory seasons up to the 10th week. It is evident how the flu positivity rate stood out this year, up to the 8th week that is, whether we compare it to the corresponding rates in the previous two years or to the Covid and RSV positivity rates.

As regards the individual positivity rates in all the samples, the 'switch' never took place in the 2023/24 respiratory season (i.e. the total number of positive Covid tests in all samples tested remained higher than the number of positive flu tests) in and occurred by the end of the 3rd week in the 2022/23 season.
SARS-CoV-2 has not been the main pathogen in samples since Week 4 this year, with 523 positive tests (6.8% of the 7,706 samples tested up to the 11th week), as influenza remains in the lead with 2,270 positive samples by week 11 (29.5% of all samples), followed by RSV (271), human metapneumovirus (HMPV, 144), rhinovirus (63), parainfluenza (7), adenovirus (6), and bocavirus (4).

Hospitalisations
274 people with severe acute respiratory infection (SARI) were hospitalised on the 11th week of 2025, of whom 42 (or 15.3%) required intensive care, with the latter showing deterioration from 34 (10.6%) in ICUs a week earlier. On the 11th week in the previous two respiratory seasons 10.5% and 14.9% of SARI patients were treated in ICUs, respectively.

The number of Hungarians hospitalised with SARI dropped by almost 15% w/w on the 11th week of 2025, compared with -38% a year ago and no change two years ago. The fluctuations have been too heavy to draw far-reaching conclusions from the weekly changes alone.

For the second time in the current respiratory season, the proportion of SARI patients with RSV was higher than that of patients with Influenza, while coronavirus has practically disappeared from the group of hospitalised SARI patients.

The following graphs show that influenza caused more problems this year than in the previous two seasons, while coronavirus did not lead to such a high proportion of hospitalisations and RVS followed largely the same pattern as last year and proved even slightly less severe since week 5. Two years ago, no SARI patient with RSV was hospitalised until the first week of 2023, but their share started off much higher.



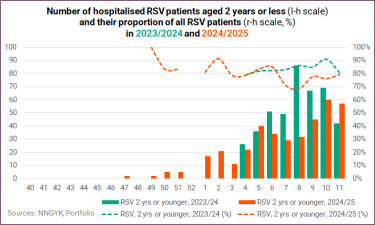
In terms of hospitalised RSV patients aged two years or younger, this season started earlier, with a few children admitted already on the 47th week, while the first hospital admissions due to RSV occurred only on the 4th week of 2024 in the previous respiratory season. As regards their share of all RSV patients, the lowest reading was 68.1% this year, while it remained north of 80% up to the 12th week last year.
Their proportion was almost 80% on the 11th week this year, with 57 of the 72 RSV patients aged two years or younger.
Age distribution of hospitalised SARI patients
Of the 274 people in hospital with SARI, 97 (35.4%) were aged two years or younger, which shows a drop from 119 (37%) a week earlier, while 106 (38.7%) were aged 60 years and older, a rise (101, 31.4%) compared to the previous week.

There were two COVID-19 patients among the hospitalised SARI patients, the same as a year ago. A year ago, of the 162 people in hospital with SARI, 84 (51.9%) were aged two or younger, while 39 (24.1%) were 60 or older. While on the 11th week of 2025, both of the coronavirus patients hospitalised were over 60 years of age, they were younger a year ago.

The age breakdown of people seeking medical help with ARI and flu-like symptoms are shown below.
The majority of ARI patients belonged in the 0-14 age group throughout the 'flu season' last year (and so far this year too), while the share of people going to the doctor with flu-like symptoms was the highest in the 15-34 age group up to the 2nd week of last year when the youngest were in majority for nine weeks and then it was back and forth between the 13th and 20th week. You fund a heat map for the previous season in one of our previous articles here.
The number and share of children up to 14 years of age remains higher among people with influenza-like illness than the number and share of those in the 15-34 age group, for the sixth week in a row, after a brief switch on the first two weeks of 2025.
Around 113,500 of people with ARI and nearly 21,000 of people with ILI were in the 0-14 age group on the 11th week of 2025. The former compares with about 100,000 a year earlier, while the latter compares with around 11,200 in the base period.


Whooping cough lingers
The number of suspected pertussis cases rose on the 10th week of 2025. Based on the figures for the first ten weeks of the year, it looks likely that 2025 will bring another record, unless a dramatic improvement occurs along the way.
The number of suspected whooping cough cases closed at an absolute record of 1,354 cases in 2024. Authorities reported 13 suspected cases for the 10th week of 2025, by which time more than 29% of the 143 cases were infants this year. Also, nearly 45% of the infections were detected in the 0-14 age group and over half in the 0-19 age group.





Cover image (for illustration purposes only): Getty Images






